Sanford Center for Aging Guidebook
Your Guidebook to the Basics of Beginning Care
- Quick Start Guide
- Introduction: Are You a Caregiver?
- Self-Care for the Caregiver
- Activities of Daily Living
- Communicating with Health Care Professionals
- In-Home Care
- Palliative and Hospice Care
- Part-Time Out-of-Home Care
- Long-Term Residential Care
- Home Safety
- Insurance
- Legal Aspects of Caregiving
- Financial Aspects of Caregiving
- Working While Caregiving
- Glossary
- List of Medications
- In Case of Emergency

Quick Start Guide
Top Ten Things to Get in Order
Self-care for the caregiver
It is easy to focus only on caregiving tasks and forget that you need to take care of yourself. Give yourself time each day to focus on your personal wellbeing.
Activities of daily living
Using the list provided in Activities of Daily Living, note what Activities of Daily Living (ADLs) your family member can do alone, what they need some help with, and what activities require a lot of help.
Communicating with health care professionals
Ask questions! Make sure all your questions are addressed.
In-home care
Know when you will need a break from caregiving (respite care) and what type of respite care you are seeking.
Part-time out-of-home care
Know which community centers have programs available for seniors. There may be recreational activities and meals that you can both participate in together.
Long-term residential care
Make a list of amenities that you and the person you are caring for would like to see in assisted living or nursing homes. Take this list with you when visiting different locations.
Home safety
Showers, bathtubs, and changes to floor level should have safety grab bars.
Insurance
Having a direct connection to the right insurance professional for support and advice is essential.
Legal aspects
Will you be the legal guardian of your family member? If so, you may need to set up a quick legal framework.
Financial aspects
Do you know your family member’s financial information? Make certain that their accounts, and your own accounts, are in order.
Introduction: Are You a Caregiver?
The caregiving experience is unique to every individual. You may live with the person you care for full-time as a spouse, partner, or adult child. You might be managing the care from a distance as a friend or neighbour. Although the type of care may be different, every type of care provided is important.
Caregiving can be rewarding, but it can also be overwhelming and it may be a hard transition in your life. The important thing to know as you go through this caregiving journey is you are not alone. Others understand what you are going through and may have helpful advice for you.
This guidebook is intended for unpaid family caregivers to seniors. It may not include everything you need to know, but it includes advice from professionals and other caregivers. The guidebook is set up in sections so feel free to skip to the sections you and the person you are caring for find most valuable. Each section has tips and advice from local caregivers.
As you read the guidebook, you may want to know about specific resources that are available. To find resources in Nevada for caregivers or seniors, visit nevadacaregivers.org, and type in a keyword to what you would like to find. A list of providers with information about qualifications and details of the services they provide will help you decide what fits your needs. The site is updated regularly and contains hundreds of specific service providers.
A Spanish version of this guidebook is also available. If you would like printed copies of the guidebook in English or Spanish, or need additional information, please contact the Sanford Center for Aging at (775) 784-4774.

Self-Care for the Caregiver
Caring for elders can be stressful both physically and psychologically. Taking on the responsibility for someone else, dealing with doctors and insurance companies, finding appropriate and affordable resources, and attending to daily meals, dressing, bathing, or even just providing company can be time-consuming, exhausting, and challenging.
Caregiver burnout
Caregiver burnout is common among caregivers. This happens when a caregiver is exhausted physically, mentally, and/or emotionally and needs immediate support and relief from caregiving responsibilities. If you begin feeling overwhelmed, helpless, impatient, and/or irritable, reach out to a friend or family member for immediate help. The following information goes over techniques for relieving stress and preserving a healthy relationship between the caregiver and the person you are caring for.
Set Realistic Goals
Do not set yourself up for failure. Know your limits and set goals that are obtainable and will make you feel good. Remember to give yourself credit for achieving these goals.
Practice Good Communication
It is important that you acknowledge your feelings and talk to someone you trust and feel comfortable with. Do not expect others to know your needs. Express them!
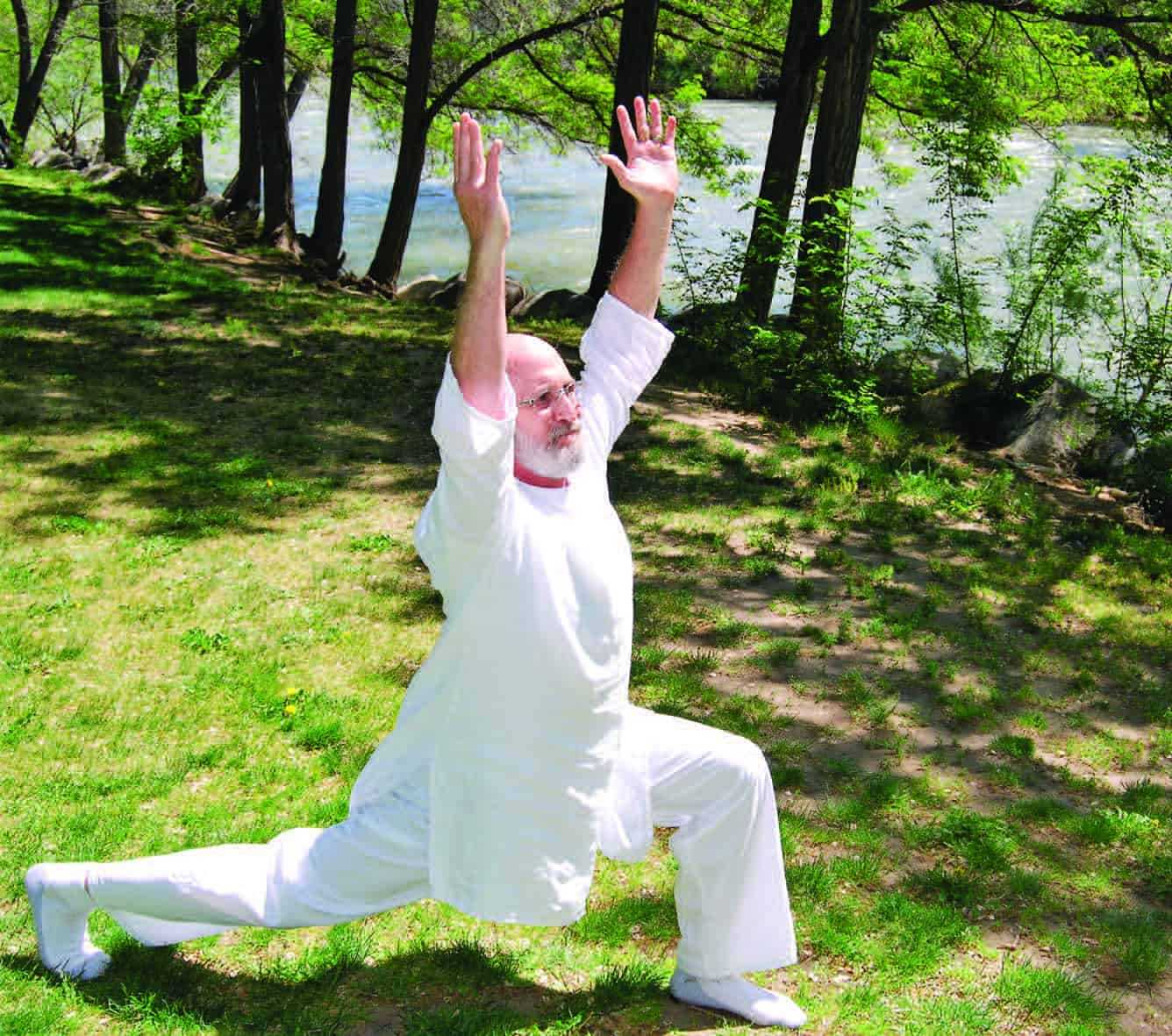
Maintain Your Health
It is important that you keep up on your own health and consider yourself. Remember to eat well, exercise regularly, sleep well, and rest a little bit every day. Participate in pleasant, nurturing activities, such as reading a good book or taking a warm bath to maintain your mental health as well.
Laugh
Laughter and humor can bring balance to your life and emotions. Keep a positive attitude, share fun stories with the person you are caring for and other caregivers, and remember to laugh at least three times a day.
Network with Other Caregivers and Family Members
Being able to identify and communicate with family members and other caregivers going through similar situations can bring a sense of relief and reduce isolation. There are many support groups available specific to medical, emotional, and physical disabilities.
Seek Information
The power of knowledge and information is key to relieving many stress factors. With increased knowledge, you can better prepare for the future and more effectively handle challenging situations. The library or internet can be great and accessible tools for obtaining information; just be cautious of where an article is coming from. Explore local resources or contact us at wellness.sca@unr.edu or 775-784-4774.
.
Promote Independence
There is a difference between caring and doing. Be open to technologies and ideas that promote the independence of your family member as long as possible.
Socialize
One of the negative impacts of caregiving is isolation. It is important to socialize with friends and/or family, start a new hobby, or return to one you enjoy. The point is to stay involved and active in things you like and that relax you.
Seek Respite Services
Respite means “time off.” Respite can be provided by a friend, family member, or by a service in the community. It can be enough time for you to take a nap, go to lunch with friends, or even enough time to go on vacation.
Form a Village
As a caregiver, it is very important that you understand that it is okay to share your work and responsibilities. Do not be afraid to accept the help that others are offering, or to delegate some of your duties. Be as specific as possible in what others can do as team players.
Activities of Daily Living
Caregiving is different for every person, but there are tips and tricks that can be helpful to everyone when dealing with everyday care. To help you further identify the needs of your family member, read through the Activities of Daily Living section and fill out the needs assessment that follows. This will help you to identify where additional help is needed. When professionals talk about “Activities of Daily Living,” they are generally talking about a senior’s ability to eat, bathe, dress, move, toilet, and maintain personal hygiene and the level of assistance needed for each activity. Like many aspects of beginning care, this is a learning opportunity. You will learn what the person you are caring for prefers, what they need help with, and how to improve their care as you try different techniques. The following sections go over some common tips for these activities.
Eating
Mealtime can be a great experience for the person you are caring for, but it can also be a stressful experience if they have difficulty eating. Being relaxed and allowing plenty of time for meals can improve this experience. Be aware of the difficulties your family member has while eating and make accommodations. If they have difficulty seeing, describe to them where the utensils, napkin, and drinks are located. If they have difficulties chewing, choose foods that are softer. If they have trouble feeding themselves, ask if you may help before you step in to feed them.
Mobility
Recognize the abilities of your family member in order to prevent falls. Notice when they begin to have more difficulty walking and what shoes are worn. Slip-on shoes or slippers increase the chance of falls. Make sure you also know when the person you are caring for needs to use durable medical equipment (DME) such as a cane, walker, or wheelchair. Speak with their primary care doctor to learn more.
Transfers are usually a large concern for caregivers. You will want to see the level of help your family member needs to transfer from the chair to bed, toilet to chair, etc. and learn how to safely assist them. It may take a professional to teach you how to transfer someone. Do not jeopardize the safety of yourself or the person you are caring for by trying to do transfers without knowing exactly how or without having the strength to perform them properly.
Bathing
The greatest number of home accidents occur in the bathroom, which is why bathing and showering are such a large concern. There are precautions you can take to make this time safer for both the person you are caring for and yourself.
- Put adhesive strips or a rubber mat on the bottom of the tub or shower to make the surface less slippery when getting in or out.
- Put grab bars inside and outside the shower or tub (see the Home Safety section).
- Use a shower bench for your family member to sit on while showering.
- Make sure you are giving the person you are caring for your full attention as they get in or out of the tub. Depending on their abilities, both physically and mentally, this may mean simple supervision or assistance.
- Do not perform any activity that could be dangerous for you or the person you are caring for. If you do not feel comfortable helping the person get into and out of the tub, ask a professional to teach you the best practices.
- Determine the best time to complete a bath or shower depending on both your preferences.
Dressing
Encourage the person being cared for to dress him or herself as much as possible. Learn when they need assistance. If a person has weakness in one side of their body, it is recommended to dress that side first (putting the weaker arm into the sleeve or the weaker leg into the pants first). You may need to assist when the person rises to finish dressing or they may need some assistance with buttons or zippers.
Toileting
Depending on the level of care needed, you may need to provide assistance with simple reminders to use the toilet, or your care may be as involved as changing an adult brief. If the person you are caring for requires minimal assistance, there are a couple of easy tips you can use to ensure that their care needs are met. Make sure that the path to the bathroom is always kept clear and well-lit at night. If they have difficulty sitting down and getting up, install grab bars and an elevated toilet seat or even a taller toilet.
Urinary incontinence is a normal part of aging. When dealing with incontinence issues, adult briefs or incontinence pads are an option depending on the severity. If the incontinence becomes more of a problem, contact a doctor. Bowel incontinence is less frequent, but if it occurs, contact a doctor for tools to help.
Personal Hygiene
Personal hygiene is important for the person you are caring for and can become difficult for a person as they age. An individual’s inability to maintain their hygiene is a sign that they are becoming less able to care for themselves. Notice if your family member is still able to brush their teeth or dentures, comb their hair, and maintain their appearance. These are indicators that they may need more assistance. If there are significant changes in their hygiene, contact their doctor, as it could be signs of a larger problem.
Needs assessment chart
Please download the PDF of this Nevada Caregivers Guidebook for a needs assessment chart. Fill out this needs assessment chart to identify the strengths of the person you are caring for and where your help is most needed.
Alternatively, identify whether the person you are caring for can accomplish the following tasks alone, with some help, or with much help.
- Bathing
- Dressing
- Maintaining personal hygiene
- Toileting
- Preparing a nutritious meal
- Eating a nutritious meal
- Getting out of a chair or bed
- Walking
- Climbing stairs
- Using the phone
- Managing medications
- Driving or using public transportation

Communicating with Health Care Professionals
The ability to talk openly with a doctor and other health care professionals is an important part of good health care for you and your family member. Effective communication includes: asking the right questions, being proactive with your concerns, and using the time you have to your best advantage. Some tools to consider when you and the person you are caring for visit a doctor’s office are listed below.
Show Respect for the Person You are Caring For
Make sure that your family member speaks for themselves if they are able to do so. Encourage them to share any physical, emotional, or mental concerns with the doctor, especially any changes in the family or living conditions which could be causing undue stress. As the caregiver, you can step in with information at an appointment if the person you are caring for forgets anything important about their health.
Make a List of Concerns
Before every visit, make a list of concerns. Prioritize what you both want to discuss. Ask about the most important things first.
Take Notes
Always take notes at medical appointments and make sure that you write down the doctor’s instructions so that you can go over what was said and done with your family member when you return home. Request a visit summary/printout if one is available. Write down the names of people who helped you and what they said.
Plan to Update Your Doctor
Let the doctor know of any changes in physical function, appetite, weight, sleep, or any other changes that you might have noticed. Make sure that the doctor and staff know if the person you are caring for is having trouble seeing or hearing and if they wear hearing aids.
Ask Questions
Asking questions is essential for good communication. Before every visit, prepare a list of questions you would like to discuss with the doctor. If you do not ask questions, the doctor may assume you already know the answer or that you do not need more information. Ask questions about anything that does not seem clear, such as when you do not know the meaning of a word or when instructions seem confusing or incomplete. There are no “dumb” questions; only unasked questions. Ask questions that will confirm your understanding. You might say: “I want to make sure I understand. Could you explain that a little more?” Do not be afraid to tell the medical professional if they have not answered your question.
Take Information with You
Take a list of all medications the person you are caring for takes and the dose (the back of this guidebook has a section to fill out a list of medications). If you are worried about forgetting any medication, take all their prescriptions with you to the appointment. You should also take their insurance cards, the names and phone numbers of other doctors and pharmacists they use, and their medical records if they are seeing a new doctor
Medication
Some medicines cause unpleasant and/or dangerous side effects. Discuss the medicines being taken. Make certain that the doctor knows how many are taken, why they are taken, and how often they are taken. Describe, or have the person you are caring for describe, any drug allergies or reactions to drugs that they may have had. If the doctor prescribes a new medication, discuss the potential side effects, the time of day it should be taken, and generic brand options. Generics are often less expensive than the original and your doctor will be able to advise you as to whether you should take the generic or original.
CARE Act
As part of the CARE Act passed by the Nevada Legislature in 2015, hospitals are required to provide the opportunity for a patient to designate a family caregiver. When a family caregiver is identified, the medical staff must inform the designated caregiver when a family member is to be discharged to another facility or back home. They must also provide the caregiver an explanation and demonstration of any medical tasks which will need to be performed at home. Make sure that you are designated as the caregiver if you will be providing care at home.

In-Home Care
There are a variety of home care services intended to support and care for seniors. With so many options, finding the right service can be a difficult task. There are various levels of in-home care services offered, including: companion care, personal care services, home health, palliative care, and hospice care. It is important to narrow down your needs and to know the resources that can help you.
Companion care and personal care
Companion care and personal care are often offered by the same agencies. These services are not usually covered by health insurance, including Medicare, but may be covered by longterm care insurance, voucher programs, and/or a Medicaid program called Personal Care Services (PCS). If not covered by insurance, these care services will require out of pocket payment. These providers are non-medical and do not assist with any type of medical treatment.
Companion Care
Companion care provides a companion who can assist with most tasks, including driving. They provide support if the one you are caring for is not safe alone.
Personal Care
Personal care meets the basic needs of an individual. Personal care staff members are certified in assistance with daily living tasks. They can prepare meals, give medication reminders, do light housekeeping, and assist with bathing and personal hygiene.
Home Health Care
Home health provides in-home medical care for homebound patients, including a variety of in-home medical treatments. Generally, this service is ordered by the hospital doctor or a primary care doctor.
Ask your doctor to order an assessment to see if your situation qualifies for home health. Based on your needs, your doctor will assign a clinical team that could consist of nursing staff, therapists, social workers, and possibly aids. The level of care provided depends on the condition, care needs, and the insurance benefits available to the person you are caring for. Health insurance benefits vary, but often cover home health care.
Home health care can often be combined with personal care services to ensure a safe transition home and full support for your care needs. Communication with the hospital case managers, the doctor, and the selected home health company is critical to ensure everyone is on the same page regarding the care needs, support systems available, limitations, equipment, and supplies needed to facilitate that care. Try to make arrangements for home health care prior to leaving the hospital.
Before Choosing an Agency or Caregiver
To decide which agency fits your needs, you will want to consider cost, certifications, specialized staff training, their communication with family caregivers, and the caregiver selection process. Once you have narrowed your search to a few agencies, call each and make sure that all your questions are answered and any concerns are addressed.
Make sure that the caregivers you hire are individually licensed or bonded in the state of Nevada. Agencies in the State of Nevada are licensed by the Department of Health and Human Services and survey results for the agencies are for public review. It is strongly recommended to review survey results before choosing an agency. Caregivers employed by an agency are required to receive training, be fingerprinted, and obtain a background check. Caregivers are supervised and the agency is responsible for the delivery of care. Always interview the person assigned to you to see if they will be a good fit.

Palliative and Hospice Care
Palliative Care
Palliative care is a way to improve quality of life for someone who is being treated for a serious illness. Palliative care providers are experts in easing symptoms that cause distress, such as pain, nausea, vomiting, anxiety, constipation, sleeping, and breathing problems. They are also experts in coordinating different care, giving information to help with decisions, and creating an advance care plan.
Palliative care is given by a team of people who focus on the physical, emotional, and psychosocial aspects of advanced illness. The team may include a palliative care doctor or nurse, social worker, spiritual advisor, and others. For palliative care to be most effective, both the patient and the caregiver play an active role.
Hospice Care
The goal of hospice is to give comfort and support to a terminally ill patient, their caregiver(s), and their family. Hospice focuses on quality of life and helps someone live his or her last days with a sense of control. Hospice programs support both the patient and family and include physical, emotional, and spiritual services.
A person with an illness can go into hospice when a health care provider believes he or she has about six months or less to live. Hospice continues as long as it is needed. If a person’s health improves, he or she can end the hospice care and start it again later.
Hospice is most commonly provided in the home. It can also be offered in the nursing home, assisted living facility, or hospital depending on the person’s care needs. Hospice care is provided by an interdisciplinary team, which includes doctors, nurses, and other health care professionals. A registered nurse (RN) case manager coordinates care provided by the hospice team.

Part-Time Out-of-Home Care
Respite care is an essential part of caregiving. It is crucial to have some time away to attend to business, medical appointments, grocery shopping, or simply personal time. Caregivers who take regular breaks have better stress regulation and improved long-term health. It is important that you stay healthy as you are giving care. Out-of-home programs can be a great opportunity for socializing for the person you are caring for and it can be a healthy respite for you, the caregiver.
Adult Day Care Centers
These programs provide respite care for the caregiver or may be needed if the caregiver is working and the person being cared for cannot be left alone. Adult day care centers offer a safe environment and provide social interaction, which is important to the well-being of both the person you are caring for and for yourself. Most centers offer full-time or part-time availability.
Long-term Care Facilities
For the much needed vacation or an emergency requiring you to be gone for a few days, there are programs that offer overnight and respite stays.
Adult day care centers and long-term care facilities charge for these services and require some planning ahead. There are scholarship funds available. Long-term care insurance policies may also cover costs. As with most programs, one size does not fit all. Review all options before you make a choice and ask for suggestions from fellow caregivers.
Homes of Other Family Members or Friends
Neighbors and friends may offer to have your family member visit while you take a break for a few hours. Reach out to trusted individuals and be honest with your need for assistance.

Long-Term Residential Care
Sometimes it is impossible for a caregiver to keep the senior they are caring for at home. If the caregiver must work full-time or cannot physically provide care, often a long-term care community is the only choice. The choice should be carefully made to ensure the senior is safe and comfortable.
Before visiting any residential care options, it is important to have a clear picture of your family member’s needs in order to know what level of assistive care is needed. Get a history and physical report from the doctor, an up-to-date medication list, and write out a list of concerns and care priorities. You will need to know things about your family member like: can they get in and out of bed on their own, can they administer their own medications and can they transport themselves if needed. Visit several different locations to find what is offered, and what suits the senior’s needs. Include the person you are caring for in the decision making as much as possible. Make certain that the residences are licensed and insured, and that the staff is appropriately trained for the level of care they provide.
Once you have found the long-term care residence that suits the needs of your family member, visit as often as possible and at different times throughout the day. Visit during meals, so that you can see what food is being offered and if there is adequate assistance. Do a drop-in visit to see what an average day looks like.
Make certain that there are familiar possessions in the room; things that your family member is used to seeing and using every day: furniture, paintings, books, afghans or blankets, and cherished items. Having personal possessions lessens the stress of not being at home. Residential care is often costly, and not covered by most health care insurance. Check with your family member’s insurance to see if coverage is available. If coverage is not available, they will need to pay for care out of their own income/assets or apply for Medicaid. The following page provides descriptions of different long-term care options. Each setting provides different levels of care.
Assisted Living or Group Homes
Assisted living or group homes provide meals and care with daily living activities, such as dressing and bathing. They do not provide nursing care and many do not have a nurse or other medical professional on staff. Assisted living locations range in size from homes with two to ten seniors being cared for to larger locations with 50 or more residents. Residents may leave freely. Assisted living often provides transportation to residents for shopping or medical appointments. It is common for seniors to be placed first in assisted living and later moved if care needs increase.
Memory Care
Memory care is a locked assisted living community providing security as well as meals and care with daily living activities. These communities provide transportation to residents for medical appointments. They often do not provide nursing care and do not have a nurse or other medical professional on staff. Residents may not leave freely and are constantly monitored to ensure their safety.
Skilled Nursing
Skilled nursing has full 24-hour medical staff including nurses and at least one doctor. Skilled nursing locations are generally large with more than 50 residents. Residents are monitored and can leave under certain circumstances. Skilled nursing provides total care and transportation for medical appointments.

Home Safety
Home modifications are changes made to the living environment to increase ease of use, safety, security, and independence.
As a caregiver, you will want to make sure your home environment is safe and that you decrease the risk of injury. Changes to the home will also make it easier for you to provide care and enhance the ability of the person you are caring for to do as much as possible, as independently as possible.
Consider the short and long-term needs of your family member. Depending on a person’s condition, changes may be temporary or permanent. For example, if your family member is using a wheelchair, plans need to be made for how to get the person in and out of the home. There are temporary ramps that can be put in place and removed when the need no longer exists.
A hospital staff person (a nurse, physical therapist, or occupational therapist) who has worked with your family member can give you valuable recommendations. If a home health agency, occupational therapist, or physical therapist will be coming to your home, they will make recommendations based on the layout of the house and the abilities of the person you are caring for.
Keep in mind that some modifications, such as better lighting or safety bars in the bathroom, are great safety devices for all residents as well as guests, no matter their abilities.
Here are some suggestions to consider:
- Understand the limitations of the person you are caring for.
- Consider your family member’s vision, mobility, and ability to perform activities (see Activities of Daily Living section) when determining home modifications.
- A person with dementia may require different kinds of safety modifications compared to someone with physical disabilities.
- Many changes can be made by you, a family member, or friend. Some modifications might be best left to contractors or handyman businesses that have experience in this area. Ask for references.
Take the following checklist and travel through your home inspecting each area, as well as the entrance/exits and garage accessibility. This is a short list and a start. Later on, you may identify other needs as the care issues become more evident.
Outside the House
- Sidewalks and curbs are free of uneven surfaces and cracks. Trees and bushes do not interfere with walking and vision.
- Access to the entrance has no steps, steps with handrails, or a ramp with handrails.
- There is adequate automatic lighting that comes on when darkness falls.
Inside the House
- Walking surfaces have low cut carpet or flooring that does not present a slipping hazard.
- There is adequate lighting throughout the house and night lights that come on in the dark, especially in hallways leading to the bathroom.
- Doorway spaces are wide enough to accommodate a wheelchair, walker, or someone assisting.
- Areas are free of clutter and sharp corners.
- Throw rugs are anchored to the floor or removed.
- Chairs, couches, and sleeping surfaces are firm and high enough to allow comfortable and safe transfers and do not have wheels or casters.
- Phone, lamp, and extension cords are out of the flow of foot traffic.
- Phone is easily accessible or mobile in case of emergency. Personal emergency report systems can also be arranged through the hospital or other providers
Bathroom
- The toilet seat is high enough to allow a person to sit and stand safely.
- The shower/bathtub has non-slip flooring and a shower hose that adjusts to sitting level.
- Bath bench is installed. Safety bars are placed by the toilet, bathtub, and shower. Towel racks are not strong enough and should never be considered a safety bar.
- Flush handle and toilet paper dispenser are accessible.
Write down any other possible safety hazards that may be present

Insurance
Knowing what medical and other services are covered by different insurances can make it easier to navigate the care system. The following is an overview of insurance issues and what the different insurances cover.
Medicare
Most seniors are eligible for Medicare.
- Part A covers hospital costs.
- Part B covers doctor’s visits, laboratory services, durable medical equipment (oxygen, wheelchairs, etc.), radiology services, and most other medical services.
- Part D covers prescription or drug costs.
You rarely pay a premium for Part A, but do pay premiums for Part B and D. Your premiums are deducted from your Social Security check monthly. If you are over the age of 65, Medicare is always your primary insurance, unless you are working and covered by employer insurance.
Medigap or Medicare Supplement Insurance
Because Medicare only pays an average of 80% of medical expenses, most seniors purchase Medigap, an insurance to pay for the balance. Contact an insurance agent, or an advocate at the local senior center or Aging and Disability Services Division office for advice on which Medigap plan is best for the person you are caring for.
Medicaid
The need for Medicaid benefits arises when a senior needs long-term care services provided at home, such as personal care assistance, or when a senior enters nursing care. Medicare only covers skilled medical care (hospitalization, post-surgical care, physical therapy, etc.). Medicare does not cover assisted daily living care (bathing, feeding, or dressing). Once a senior is admitted to nursing care and they do not require skilled medical care, Medicare stops paying for the senior’s care. It is then necessary for the senior to either pay for the nursing care out of her own income/assets or apply for Medicaid. Many seniors are unable to pay out of pocket for nursing care and will need Medicaid. In order to receive Medicaid benefits, certain income/asset qualifications must be met. Do not make assumptions about what needs to be in place to qualify for Medicaid. Call an elder law attorney, a social worker, or the Medicaid office to receive more information.
Legal Aspects of Caregiving
It can be confusing to try to understand the different legal aspects of being a caregiver. The following pages explain some common legal information you will want to talk about with the person you are caring for. You will want to contact an elder law attorney directly to get more information. These topics can be difficult to talk about with the person you are caring for, but it is important to have these forms in place.
Advance Directives
An Advance Directive is used as an umbrella term for any document that directs health care for a patient, including such decisions as whether to intubate, resuscitate, or perform other medical procedures. Health care providers have a duty to record and maintain your Advance Directive documents in your medical records. Living Wills and Durable Powers of Attorney for Health Care are all Advance Directives.
Living Will or Directive to Physician
A Living Will or Directive to Physician is a form detailing a person’s wishes for medical treatment in the case that they are no longer able to communicate their wishes themselves. This could involve withdrawing life-sustaining treatment if the person is terminally ill or in a persistent coma. Only the individual themselves has the right to execute or revoke their living will.
POLST or Physician Order for Life Sustaining Treatment
A POLST form specifies a person’s wishes about certain medical treatments they want towards the end of life. The POLST form is designed to ensure that seriously ill patients can decide with their doctor, Advance Practice Registered Nurse (APRN) or Physician’s Assistant (PA), what treatments are most appropriate. Medical orders are written based on these decisions and the orders are to be honored by medical providers including emergency services. POLST forms are available from doctors, hospitals, and hospices.
Durable Powers of Attorney
A Durable Power of Attorney appoints someone, such as a spouse or adult child, to make decisions for an individual when they are unable to do so themselves. Durable refers to a specific clause in the Power of Attorney stating that the Power of Attorney does not terminate when someone becomes incapacitated or incompetent. There are two types of durable powers of attorney.
- Durable Power of Attorney for Health Care: A Durable Power of Attorney for Health Care does more than a Living Will or Directive to Physicians. The Durable Power for Attorney appoints someone to ensure that health care wishes are followed. Family members, even a spouse, have no legal right to order health care unless appointed by the individual who is being cared for or by being appointed their Guardian by a court. Nevada has a statutory Durable Power of Attorney for Health Care form that can be found at most hospitals and in our Important Documents.
- Durable Power of Attorney for Finances or General Durable Power of Attorney: A Durable Power of Attorney for Finances or General Durable Power of Attorney appoints someone to manage the finances and property when the person being cared for is unable to do so themselves. A General Durable Power of Attorney does not allow the person appointed to make health care decisions unless the Power of Attorney specifically includes a health care clause. Most General Powers of Attorney are not durable and cannot be used if the person being cared for is incapacitated or incompetent. Nevada has a statutory Durable Power of Attorney for Finances form that is available in our Important Documents.
Document safekeeping
Copies of the Durable Powers of Attorney should be given to the individual’s agent(s). Copies should also be kept in an envelope on the refrigerator or another location where the copies are easily accessible in case of an emergency. Your doctors should be given copies of your Durable Power of Attorney for Health Care.
Wills and Trusts
Wills and Trusts designate someone to manage an individual’s estate after they are deceased and direct distribution of their assets after their death. Wills are probated (approved by the court as valid). A Living Trust, also known as a Family Trust, Revocable Trust, Irrevocable Trust, or Inter Vivos Trust, distributes your assets without probate but is more complex and expensive than a Will. Trusts are not probated unless contested, done incorrectly, or assets are not held in the name of the Trust. To find out which is best for the person you are caring for, contact an elder law attorney or your local senior center for a legal aid attorney
Financial Aspects of Caregiving
To best understand your and your family member’s needs and goals, sit down with the person you are caring for as soon as possible to discuss how much assistance they will need financially. These conversations may feel uncomfortable, but they are important to have as soon as possible to avoid costly mistakes in the future.
A financial professional may be able to advise you on how to plan for your financial future as a caregiver and for the finances of the person you are caring for. They will be able to sort out your immediate needs and concerns and help to plan for your future. If you intend on using a financial professional, make sure they have Series 7 and Series 66 licenses.
If you decide to manage your family member’s finances, it is important that you know where the following information is for your family member and keep it all in a safe place. A financial professional will ask for this information as well.
- List of existing savings
- Bank account information
- Insurance policies
- Any accrued debt (mortgage, credit cards, loans)
- Social security number
- Trust and/or will
- Durable power of attorney
- Tax returns
- Safety deposit boxes
- Medical directive
- Deeds to land
Working While Caregiving
Balancing both work and caregiving is a difficult challenge. Caregivers often feel like they are neglecting their work or neglecting the person they are caring for. Maybe you are in a similar situation and you are struggling to find a healthy balance in caring for your family member while still being satisfied with your working life.
As you are working, there will be times you need to leave early to bring the person you are caring for to a medical or dental appointment, or you might have to leave unexpectedly for a family emergency. This can be frustrating for both you and your employer. Here are a few tips to try to alleviate this stress in the workforce:
- Learn your company’s benefits and policies about caring for family members.
- Talk to your boss about your caregiving situation. This will help your employer to understand your situation further, and will give you the opportunity to ask how you should communicate with them in case of an emergency when you would need to leave work.
- Ask other co-workers that have been caregivers if they have suggestions on how to manage working and caring. Communicating your needs with coworkers will also help to create more of an understanding if you are not as present at work.
- Create a backup plan with family and friends. Sometimes you will not be able to leave work right away or an in-home caregiver may suddenly become unavailable. For instances like these, a written plan with alternatives and phone numbers is essential.
- Know your rights as an employee. You cannot be discriminated against because of your caregiving role.
Family and Medical Leave ACT (FMLA)
The Family and Medical Leave Act (FMLA) allows an individual to take up to 12 weeks unpaid leave for caregiving for a family member. This can provide relief for those who are caring for someone who has a serious health condition. There are certain requirements to qualify for the FMLA, including the size of the company. Find out what your company provides and if you would qualify. If you need time off at any point for an emergency involving the person you are caring for, you may be able to apply for FMLA.
Glossary
Advance Directive
An umbrella term for any document that directs health care for a patient and legally appoints someone to act for the patient when they can no longer act for themselves.
Assisted Living
Residential living that provides meals and care with daily living activities, such as dressing and bathing
Burn-out
What happens when a caregiver is exhausted physically, mentally, and/or emotionally and needs immediate support and/or relief from caregiving responsibilities.
Caregiver
A family member or paid helper who regularly looks after a child or an elderly individual who is sick or has a disability.
Companion
Someone who will stay with another person. Companions do not provide personal care.
Dementia
There are multiple types of dementia, some of which can begin earlier than 60-years-of-age. People with dementia show marked personality changes; have impaired reasoning, paranoia, and/or combativeness; and have memory loss. It is a chronic, progressive disorder of the mind, which can have a slow process, or which can come on quickly. The most common types of dementia are Vascular Related Dementia (associated with heart conditions) and Alzheimer’s (often inherited).
Grab Bars
Safety bars installed to allow people to get in and out of the shower, or get on and off a toilet. These are available in most hardware stores.
Grooming/Personal Hygiene
Being able to brush one’s teeth, comb or brush one’s hair, take a bath or shower, and dress oneself.
Hospice Care
Hospice care is advised by a patient’s doctor when the patient has an illness which cannot be cured or modified with current known medical treatments. The goal of hospice is to give comfort and support to a terminally ill patient, their caregiver(s), and their family.
Incontinence
When someone loses the ability to control his or her bladder or bowels.
Mobility
The ability to move without assistance. People with dementia slowly lose their mobility and become more dependent as the dementia progresses.
Memory Care
Locked assisted living community for seniors with memory problems.
Ombudsman
A state official appointed to investigate an individual’s complaints against a hospital or care facility.
Out-of-Home Care
Caregiving performed in a caregiving facility or another home, other than the caregiver’s home.
Palliative Care
Treatment prescribed by a doctor which alleviates the symptoms of a chronic or terminal illness.
Respite
A break from caregiving responsibilities
Sandwich Generation
The generation responsible for caring for their own children and for the care of an aging family member.
Self-care
Caring for one’s self, while caring for someone else. Self-care is very important in keeping the caregiver healthy
Skilled Nursing Care
Provides 24-hour medical staff that provides total care for seniors.
Sundowning
A progressive decline of mental awareness during the day. Someone who struggles with sundowning is alert at breakfast, but struggles with cognitive difficulties later in the day.
Transfer/transferring
Moving a patient from a wheelchair to a bed, toilet, or tub, and back to the wheelchair.
List of Medications
Name:
Date of Birth:
| Drug Name | Dose | Frequency Taken | Prescribing Doctor |
|---|---|---|---|
Date Compiled:
Allergies:
Primary Doctor:
- Phone:
List of Medications
Pharmacy:
- Phone:
In Case of Emergency
Full name of person being cared for:
Date of birth:
Caregiver’s full name:
Phone number of caregiver:
Name of primary doctor:
Phone number of doctor:
Name of local hospital:
Allergies to medications:
Does the person being cared for have:
- A Durable Power of Attorney for Health Care?
- A POLST and/or Advanced Directive form?
- A Do Not Resuscitate document?
Insurance:
Medicare #:
Medicaid #:
Private Insurance (name and policy #):
Other Family member’s name to contact:
Relationship to the patient:
- Phone number:
A Special Thank You
This guidebook was created by volunteers from the Community Foundation of Northern Nevada’s Caregiver Support Initiative Steering Committee. Many of the authors are current caregivers or have been caregivers in the past.
We would like to thank the following individuals on our committee for volunteering their time and expertise to write and edit the guidebook:
- Anna Aguirre
- Chris Askin
- Gay Brown
- Mary-Ann Brown
- Laura Coger
- Ginny Harding-Davis
- Marie Gibson
- Terry Henner
- Honor Jones
- Kelley Macmillan
- Teresa Mentzer
- Jean Myles
- Lora Myles
- Nettie Oliverio
- Anna Olsen-Figueroa
- William Palmer III
- Bonnie Read
- Diane Ross
- Tod Sherman
- Margaret Stewart
- Dave Stockman
- Nick Tscheekar
- Larry Weiss
We would also like to thank the other members of our steering committee for their enthusiastic support and passion for this initiative:
- Marie Baxter
- Karen Barsell
- Mary Brock
- Jennifer Carson
- Donna Clontz
- Amy Dewitt-Smith
- Christine Fey
- Shelby Grana
- Jane Gruner
- Tom Koziol
- Joanne McAfee
- Jim Pfrommer
- Peter Reed
- Anne Sigurdson
- Lorna Tobiasson
The Sanford Center for Aging at UNR Med works to enhance the quality of life and well-being among elders through academics, translational research, and outreach. For information about the Sanford Center and its programs, visit https://med.unr.edu/